
When we change the conversation, we change perceptions
In the last decade, a considerable amount of research has significantly extended our understanding of the impact of hearing loss on quality of life. We must use this knowledge and change the way we talk about it.
Hearing is a remarkable sense from many different perspectives. It serves multiple purposes in that it is the ‘social sense’ connecting us to other people through language and communication, it is the ‘unconscious sense’ by 24/7 monitoring our environment 360 ° around us and it is the ’emotional sense’ in that it controls our emotions through perceiving emotional messages of speech, as well as through music appreciation and the like.
Unfortunately, hearing is also a significantly under-valued sense as we often relate hearing or ‘not-hearing’ only to hearing sound, whether it be a bird singing, a whisper or a conversation, but hardly ever consider how hearing or not-hearing relates to and impacts the quality of our lives.
Perception of hearing loss warped by history
We often compare hearing loss to vision loss and wonder why a hearing instrument isn’t a fashion device like glasses are. I think part of the answer to this question is that people have a very different association with vision loss and hearing loss. Vision and vision loss, i.e. people wearing glasses, have been associated since the mid-ages with being literate, a scholar, and highly intelligent while hearing loss has been associated with being intellectually disabled or less intelligent.
Over centuries, people with hearing loss were put in the category of “deaf and dumb”. They were legally “entmündigt” (i.e., incapacitated) and had no social rights. In my view, one way of changing this association of hearing loss is by raising awareness about the importance of hearing well and the impact of hearing loss on personal well-being and quality of life.
We know better today
In the last decade, a considerable amount of research has been conducted which has significantly extended our understanding of the impact of hearing loss on social integration, associated health conditions and hearing benefits beyond ‘hearing soft sounds’ and ‘understanding speech’.
Research has shown that when counselling people with hearing loss, it is not only important to discuss specific ‘hearing and speech’ related aspects in social communication situations, but also to address topics such as the ‘listening effort and fatigue’ which might be experienced in these situations. People can often compensate for a hearing loss, especially a mild one, by increasing attention and focus, but it can come at a price – increased listening effort to participate in social settings. Until recently, if someone complained of fatigue at the end of the day or feeling exhausted after a social event, we didn’t associate it with increased listening effort due to reduced hearing but attributed it to other causes, like getting older. Now we know better.
Furthermore, research has also shown that hearing loss impacts one’s ability to participate socially and this has a ripple effect. For example, it can potentially result in social isolation and reduced participation in activities of daily living. This not only affects the person with hearing loss but also their significant others, family and friends, impacting quality of lives for all involved.
Hearing loss does not exist in isolation
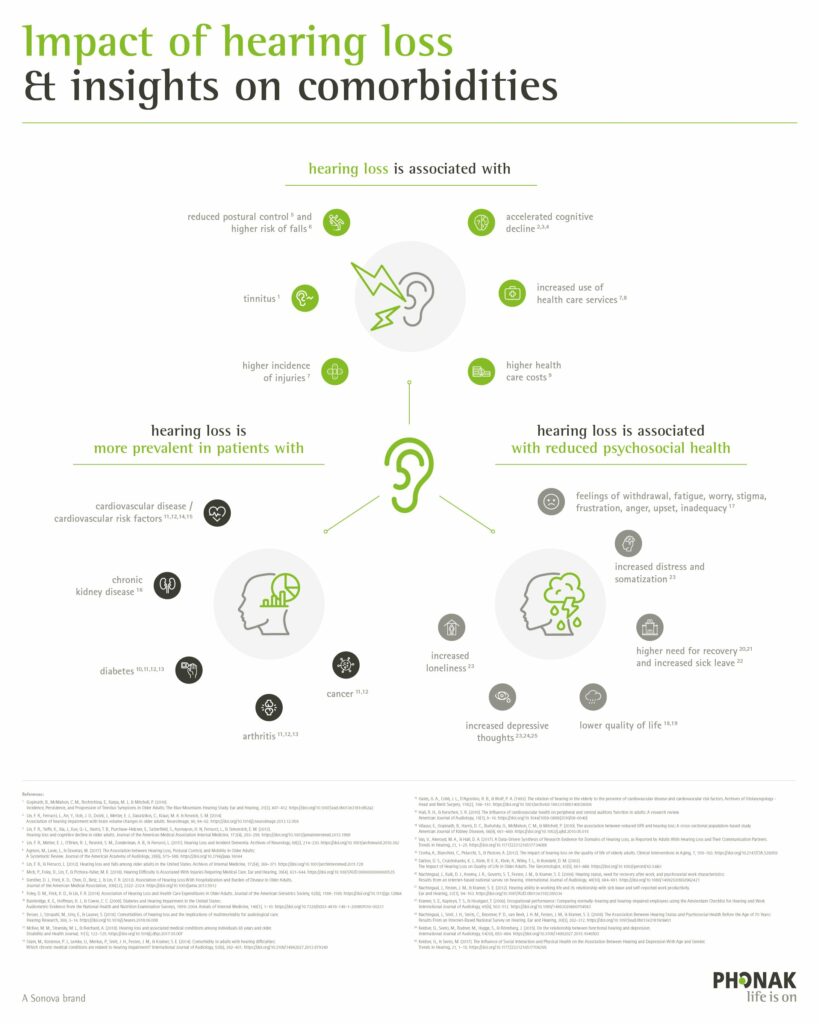 Today, science is taking different perspective of hearing loss, putting it into a more holistic context. Thanks to the availability of large electronic medical databases, big data has enabled researchers to correlate the occurrence of hearing loss with other health conditions in older adults. Some remarkable and very interesting associations were revealed when analyzing these data sets.1
Today, science is taking different perspective of hearing loss, putting it into a more holistic context. Thanks to the availability of large electronic medical databases, big data has enabled researchers to correlate the occurrence of hearing loss with other health conditions in older adults. Some remarkable and very interesting associations were revealed when analyzing these data sets.1
One particularly interesting, and potentially also causal, correlation is between hearing loss and cognitive decline. People with hearing loss seem to have a significantly higher risk of cognitive decline than people without hearing loss. Research is still not entirely clear but evidence exists that hearing loss is at least a precursor and potentially also a causal contributor. Early and consistent use of hearing instruments could be a strategy to reduce this risk.
So when identifying a hearing loss, hopefully as early as possible, it would be warranted to also counsel about potential risks related to untreated hearing loss, such as cognitive decline. This may motivate people to treat their hearing loss earlier.
Other comorbidities (health conditions that are strongly correlated with each other) for hearing loss have been found. The occurrence of hearing loss has been strongly correlated with the occurrence of i) Type II diabetes – a form of diabetes which often occurs in older adults; ii) cardio-vascular problems; and iii) a significantly increased risk of falls.
For these conditions, hearing instruments certainly are not a means to rehabilitation or disease management, but considering that miscommunication occurs in approximately 1/3 of all communication situations between a physician and a person with hearing loss, it might be helpful for these patients to check their hearing to ensure optimal physician-patient interactions.
Time to change perceptions of hearing loss
Taken together, I think it is time to put hearing loss and also hearing instruments in a very different context beyond the dimensions of ‘hearing sounds’ and ‘speech intelligibility’. We should put hearing and hearing loss in a much broader context, highlighting its importance for and impact on personal well-being and quality of life. Hearing well contributes significantly to personal well-being, well-being of significant others and healthy aging. I think in our discussions about “hearing loss” we have to communicate the impact of hearing loss on quality of life and emphasize this correlation much stronger. By doing so, we will change outdated perceptions.
If you’d like to learn more on these topics, I invite you to read an article that was recently published in Hearing Research.
Reference:
1 Besser, J., Stropahl, M., Urry, E., Launer, S. (2018). Comorbidities of hearing loss and the implications of multimorbidity for audiological care. Hear Res. 2018 Nov;369:3-14.
