The masking dilemma revisited
The challenges of communicating during the pandemic are constantly evolving. These tips can help persons with hearing loss remain safe and socially engaged during what we now refer to as ‘the new normal’.
We have all recently learned much about coronavirus, one of the major pathogens that primarily targets the human respiratory system. A unique characteristic of this virus is the route of transmission through droplets ejected from the mouth when speaking, coughing or sneezing. Multiple studies have demonstrated that speaking actually produces more droplets than does coughing (Chao, et al., 2009).
While smaller, droplets emitted when raising one’s voice are large enough to carry respiratory pathogens. Further, louder speech creates a relatively larger quantity of droplets (Anfinrud, Bax, Stadnytski, et al., 2020). Another unique COVID characteristic is that older adults are highly susceptible to the disease and are at higher risk for fatal consequences. The risk of mortality from COVID 19 increases from 3.6% for people in their 60s to 14.8% for those 70 years of age and older (Oxford COVID ‐19 Evidence Service, 2020). Older adults with co-morbidities including cardiovascular disease and diabetes are most vulnerable to COVID-19.
Often ignored, hearing loss with its associated communication challenges is a co-morbidity from which older adults being treated for COVID-19 suffer. To limit droplet spread important containment strategies during the pandemic include mass masking and social distancing. Face masking, is considered a public health intervention to intercept the transmission of the COVID-19 virus. The correct use of masks requires that the nose and mouth be covered. The mask should be tightly secured to minimize gaps between the face and the mask.
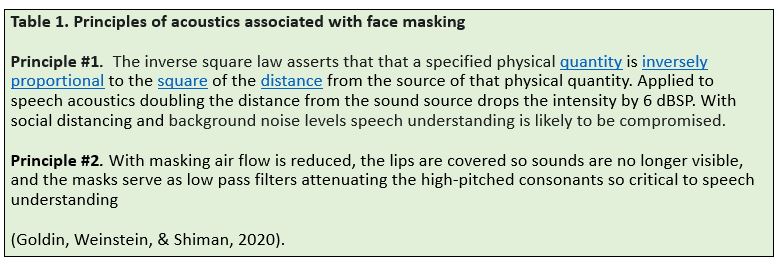
Since safeguarding with a face mask is not a guarantee (e.g. if the mask is not air tight air will leak through the sides) social distancing is an additional precaution to be taken even when wearing a mask. The rule of thumb is that individuals should maintain a distance of six feet from people with whom they are speaking. Absent a vaccine, masking and social distancing are the mechanisms available to slow the spread of the virus right now. These two approaches are anathema to what we know about speech acoustics and speech understanding (Table 1) especially for older adults at greatest risk of both COVID-19 and age-related hearing loss (ARHL).
While principle number one is well understood and is the basis for many of the communication strategies we typically recommend, a brief comment regarding principle number 2 and speech acoustics pertains. Vowel and consonant sounds are all formed in the passages of air through the throat and the mouth. Most of the energy in speech is produced in the lower frequencies and not all frequencies are essential to speech intelligibility. The frequencies which are easiest to hear (higher in intensity) are the low frequency vowels, whereas the consonants, which are higher in frequency (lower in intensity) are more difficult to detect. Simply put, there is a mismatch between the energy in the speech sounds and the import of these sounds to speech intelligibility.
Consonant sounds that appear before or after vowels help differentiate the word being spoken. In addition, not all consonant sounds are created equal, so that the consonant sounds which are the softest and are highest in frequency are the most difficult to hear BUT are the most visible on the lips. The consonant /p/ is a perfect example.
The visual modality (e.g. the ability to see the p being produced by the lips) supplements the auditory modality for sounds which are difficult to hear contributing to speech intelligibility. Since consonant sounds are crucial to speech intelligibility, when they can no longer be heard or seen, speech understanding and communication accuracy suffers.
Older adults, as we know, tend to lose their hearing for high frequency sounds and whether or not they are aware they derive considerable information from the visual modality. While hearing health care professionals are aware of the detrimental effects of face masking as relates to speech understanding, the general public and health care professionals are not tuned in to the collateral effects.
COVID-19, communication and masking
The variety of medical and non-medical face masks is on the rise as is demand. The efficiency and effectiveness of each in terms of the transmission of the COVID virus and transmission of speech sounds varies, as well!! The Alango Technologies team based in Israel and I were interested in the potential challenge to a listener’s comprehension posed by the variety of face masks currently being worn by healthcare providers. We decided to quantify measured voice samples in an anechoic chamber as a function of the type of mask being worn ranging from a simple mask to the N95 mask. While not surprising, our results were indeed unsettling.
In general, medical face masks essentially serve as a low-pass filter, attenuating the high frequencies (2000-7000 Hz) spoken by the wearer and so essential to speech understanding. A simple medical mask attenuated sound by 3 to 4 decibels whereas with the N95 mask the level of degradation was close to 12 dB. To overcome the loss of intelligibility posed by masks individuals and companies are creating masks with clear plastic so that the mouth is more visible. Demand is great among hearing health care professionals and we are now studying the differential effects of the variety masks worn by lay people and hearing health care professionals especially those which are transparent.
Communication in health care settings during the COVID pandemic and beyond
It is clear that the infective respiratory droplets generated when a person speaks, coughs or sneezes, has introduced a series of medical challenges for persons with hearing loss. In turn the widespread use of masks, the need for social distancing to help mitigate the spread of the virus, and the necessity to self-isolate have had significant downstream consequences for the health care system in general and for persons with hearing loss in particular. ED triage, inpatient (ICU) triage, and incident (multicasualty) triage protocols for example, are impacted by the need for masking and social distancing when speaking with patients/survivors of COVID-19 typically unaccompanied by family members.
In addition to speech quality degradation posed by masks, older adults who use hearing aids have commented that it is difficult to wear hearing aids, masks, and eyeglasses simultaneously. During the pandemic older adults who are being treated in hospital settings are often ‘unaided’! While data are not available, anecdotal reports suggest that loss of hearing aids is on the rise and going forward we may see a resurgence of custom hearing aids to minimize loss and damage risks!! It is noteworthy that health care providers are not immune to the challenges posed by masking and social distancing as many physicians are older and suffer from hearing loss which in many cases goes untreated/unrecognized impairing their ability to understand what their ‘masked patients’ are saying! Some suggestions to ease some of the challenges posed by our ‘new normal’ are discussed below.
Communicating with family members and healthcare providers while wearing masks and when social distancing
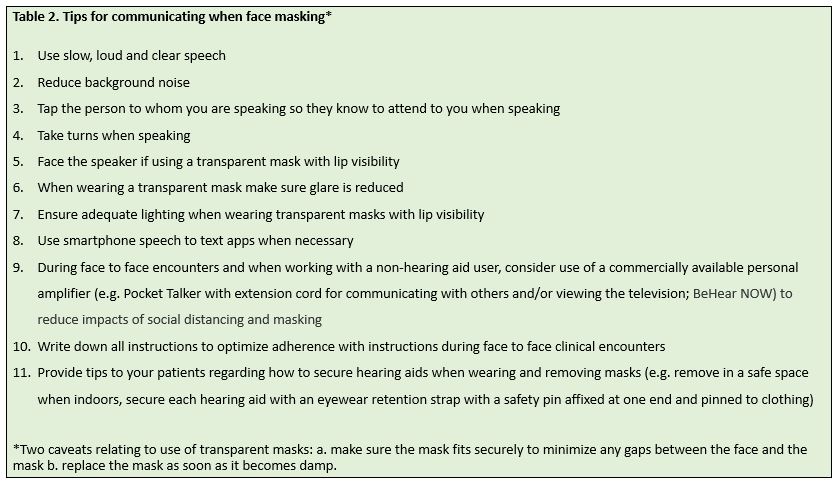
Persons with hearing loss are forced to compensate and work significantly harder to communicate because of the downstream impacts of masking and social distancing. Most of the tips listed in Table 2 are obvious and will help reduce some of the listening effort required when “masking.” I have included adaptations to consider when wearing transparent masks with lip visibility. Note that a variety of clear masks are being produced because of the high demand, but, there are only a few FDA approved medical masks with clear windows which are currently commercially available.
Concluding remarks
In conclusion, it is clear that speaking is a major mechanism of virus transmission, and wearing some form of mouth cover and strict adherence to social distancing could significantly decrease the transmission rate thereby helping to contain the pandemic until a vaccine becomes available. As hearing health care professionals we have an obligation to help persons with hearing loss remain safe and socially engaged during what we now refer to as ‘the new normal’. Going forward we should encourage hearing aid users to wear their hearing aids in all settings despite the inconvenience introduced by masking. To help optimize social connectedness and well-being, a portion of each clinical encounter should include a discussion of tips for optimizing communication (Santini, et al., 2020).
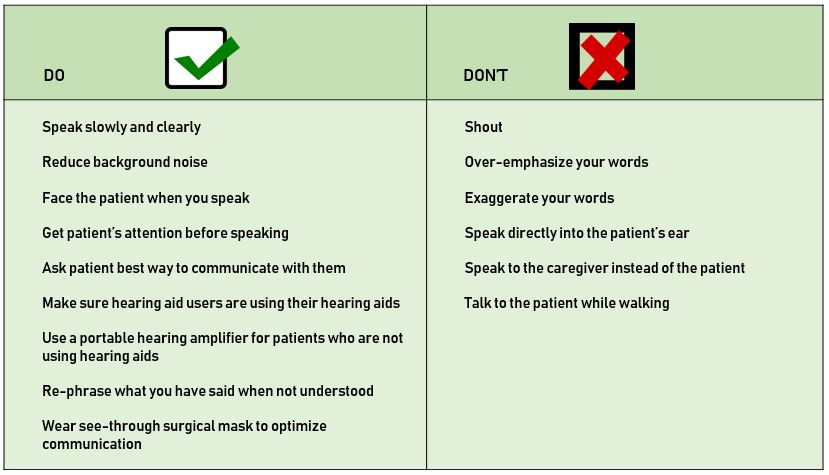
Finally, we have a professional obligation to educate health care professionals about the undesirable outcomes which attend communication inaccessibility (e.g. risk of medical misdiagnosis, hospital complications, lengthier hospital stays, lower post-discharge adherence) and to encourage posting of a ‘universal communications precautions’ document in healthcare settings which lists the DO’s and DON’Ts of effective communication as shown in Figure 1 (Mormer, et al., 2017). The challenges of communicating during the pandemic, be it verbal, written or electronic are constantly evolving. What remains the same is the need for humans to communicate responsibly and effectively.
References
Anfinrud, P., Bax, C., Stadnytski, V. & Bax, A. (2020). MedRxiv. Preprint doi: https://doi.org/10.1101/2020.04.02.20051177.
Chao, C., Wan, M., Morawska, L., et al. (2009). Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. Journal of Aerosol Science. 40:122-33
Goldin, A., Weinstein, B., & Shiman, N. (2020). How do medical masks degrade speech reception? Hearing Review. 27: 8-9.
Mormer, et. al. (2017). Hearing and Health Outcomes: Recognizing and addressing hearing loss in hospitalized older adults. Seminars in Hearing. 38: 153–159.
Oxford COVID ‐19 Evidence Service (2020). Global COVID‐19 case fatality rates. Retrieved from: https://www.phc.ox.ac.uk/covid-19/evidence-service/reviews/global-covid-19-case-fatality-rates
Santini, Z., Jose, P. Cornwell, E. et al., (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. 5: e62-e70.
We invite you to read a recent interview with Professor Barbara Weinstein on hearing health and social connectedness.