
How to build effective teams in early intervention
The way we work with a child who is deaf or hard-of-hearing and their families can influence the child’s outcomes. Collaboration and capacity building teamwork are key ingredients for success.
Research clearly demonstrates the importance of early identification, early and appropriate amplification, and early intervention for children who are born deaf or hard-of-hearing (DHH).1
From the point of diagnosis onwards, families begin building their child’s support team. In the Australian context, this tends to minimally include at least one pediatric audiologist, an ear nose and throat specialist (ENT), a pediatric speech pathologist and / or a teacher of the deaf.
Over the coming years, the child’s team will change as other medical, allied health and education professionals move into and out of the team. No matter the size or make up of the team, families are suddenly meeting lots of people and making lots of appointments. All while navigating life with a new baby and a whole lot less sleep!
Hearing and communication service providers, including pediatric audiologists and speech pathologists, are important members of the team for children who are DHH. The way we work can significantly influence how a child who is DHH, and their family, engage with early intervention, which in turn, can influence the child’s outcomes.
Best practice for teamwork in early intervention
In 2015, Reimagine Australia (formerly Early Childhood Intervention Australia) published a set of Best Practice Guidelines, which identified four quality areas, and eight best practices for early intervention. Quality Area 3 focuses on teamwork, and more specifically, on the importance of collaborative teamwork that builds the capacity of the child, family, professionals and community through coaching and collaboration.2
So, how do we do this?
The practice continuum below shows some of the main approaches to ‘teaming’ beginning with less collaborative approaches and ending with more collaborative approaches. By understanding the strengths and challenges of each model, service providers can make informed decisions about how to build effective teams for the children and families they work with.
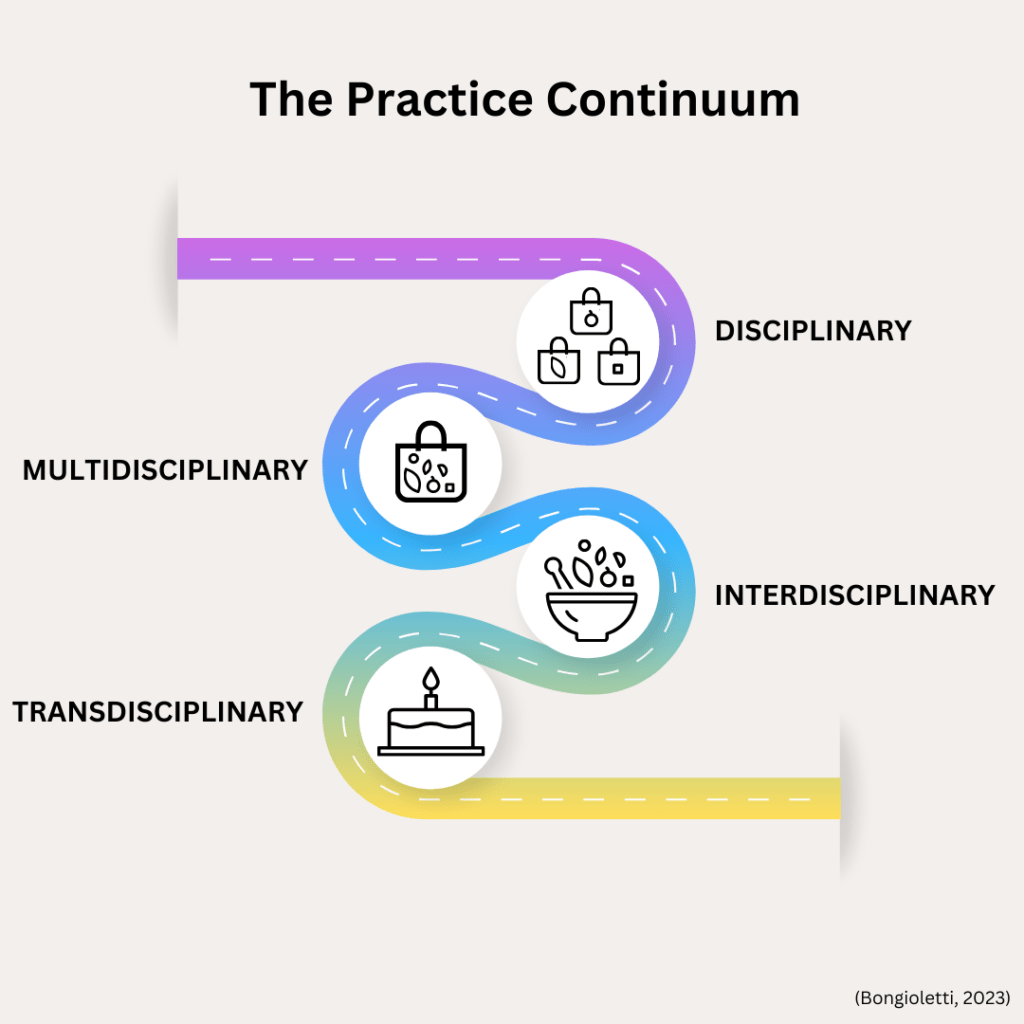
Let’s take a look at each of model of practice at a glance.
Four models of ‘teaming’ in early intervention
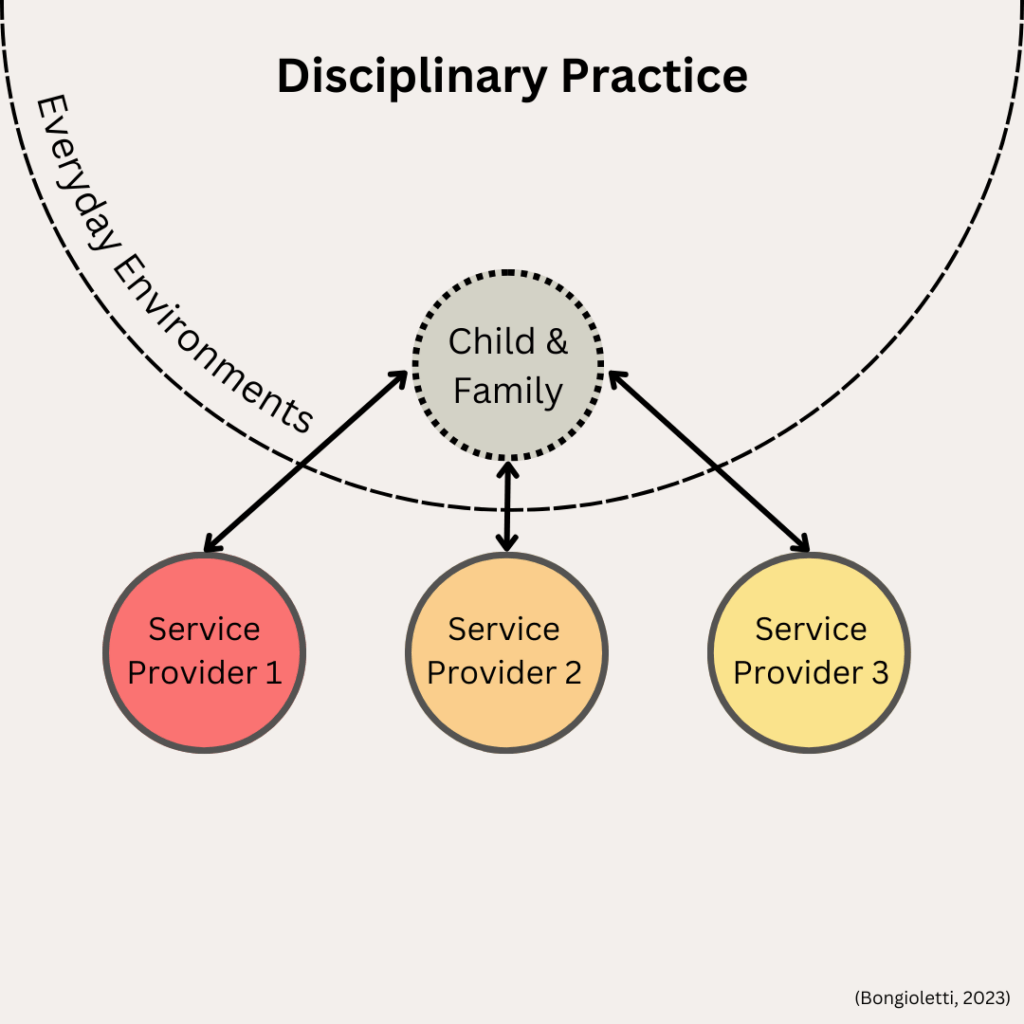
1. Disciplinary Practice is where the child and family have a separate relationship with each of their service providers, there is little to no communication between providers and no shared goals. Providers work within their discipline and are usually not aware of what other providers are working on. For a child who is DHH and their family, this might look like seeing an audiologist, speech pathologist and ENT specialist who work for different organizations – the onus is on the family to maintain relationships with each provider.
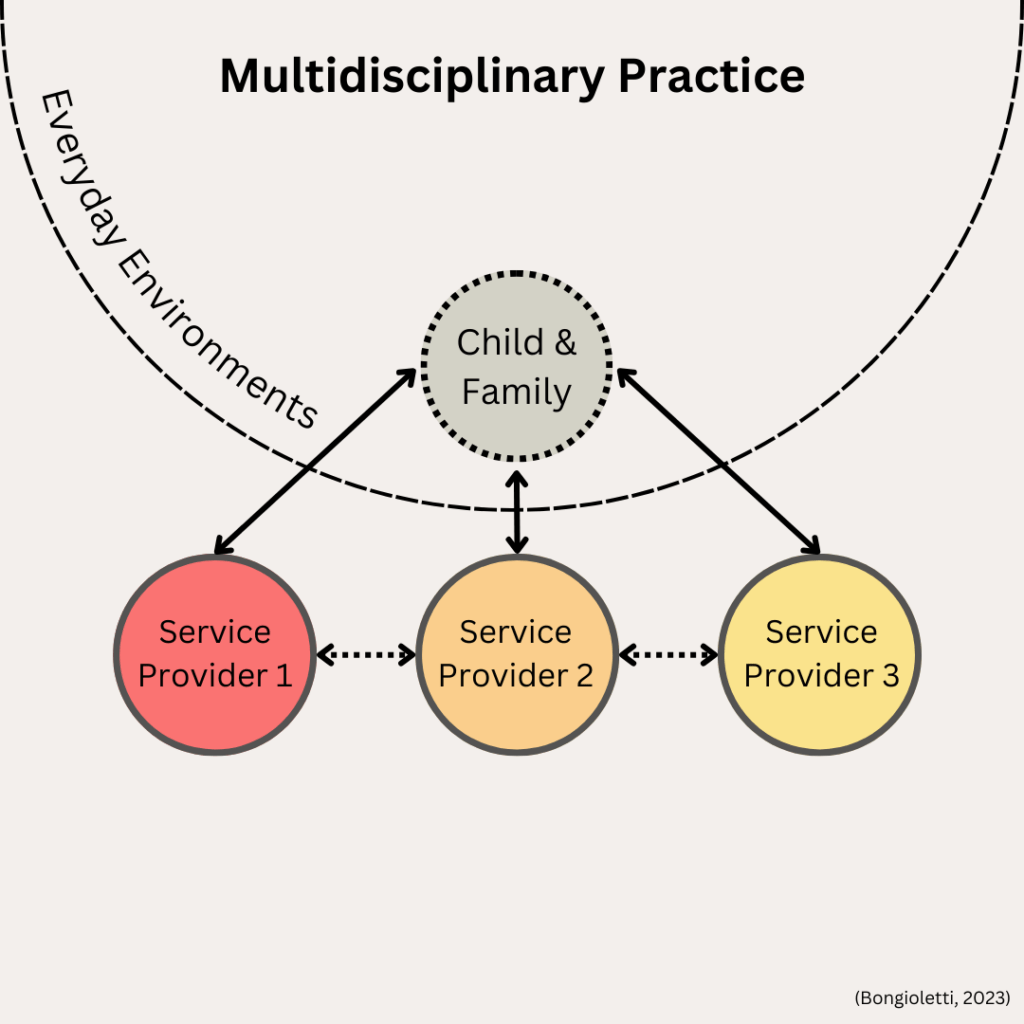
2. Multidisciplinary Practice is where the child and family have relationships with each of their service providers, there is some communication between providers, and goals are not usually shared. While providers might be aware of what others are working on, each works on their own set of discipline-specific goals. There is a sense of collaboration between team members, but the onus is still on the family to maintain relationships with each provider.
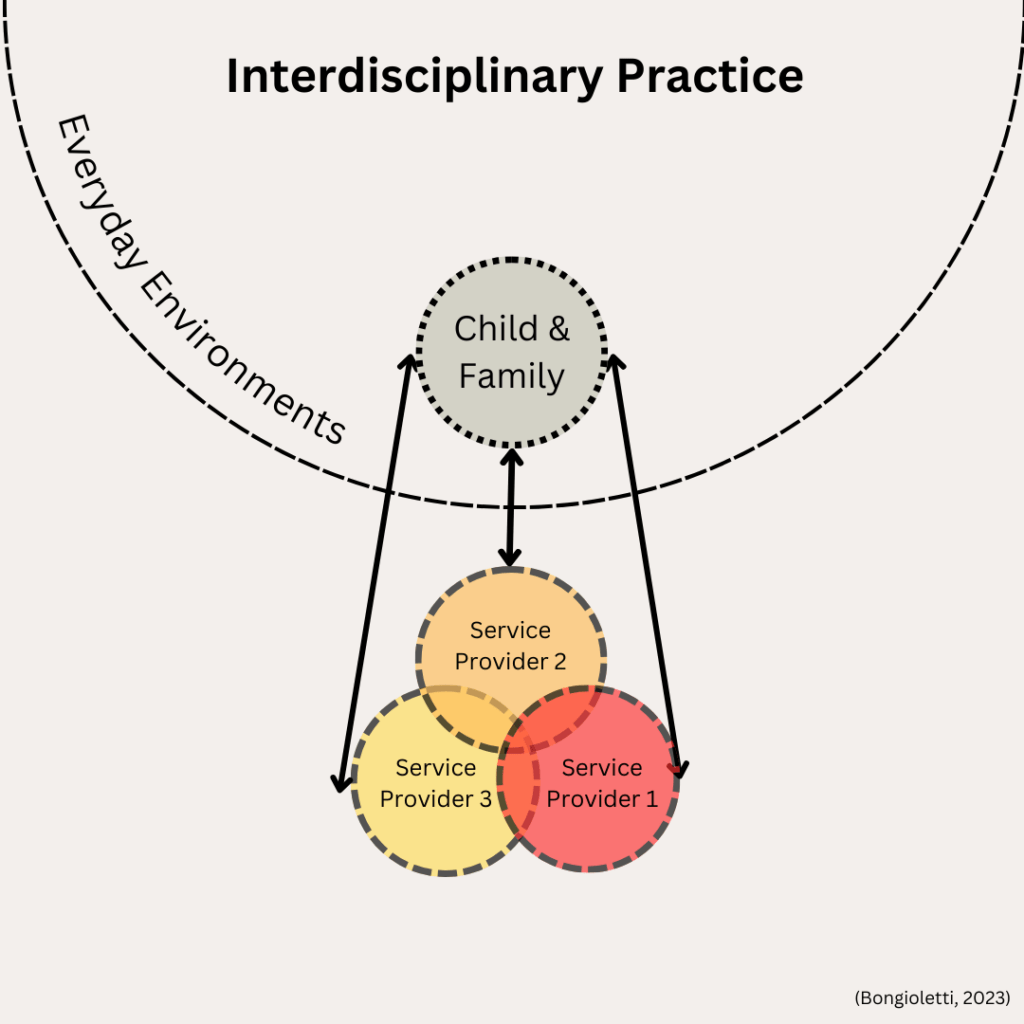
3. Interdisciplinary Practice is where the child and family have separate relationships with each of their service providers, but this time, providers communicate and collaborate with one another. Goals may be shared and addressed by more than one provider at a time, joint appointments may be conducted to address goals more holistically with input from relevant team members. While families maintain relationships with all their providers, the level of collaboration and communication allows for more holistic care.
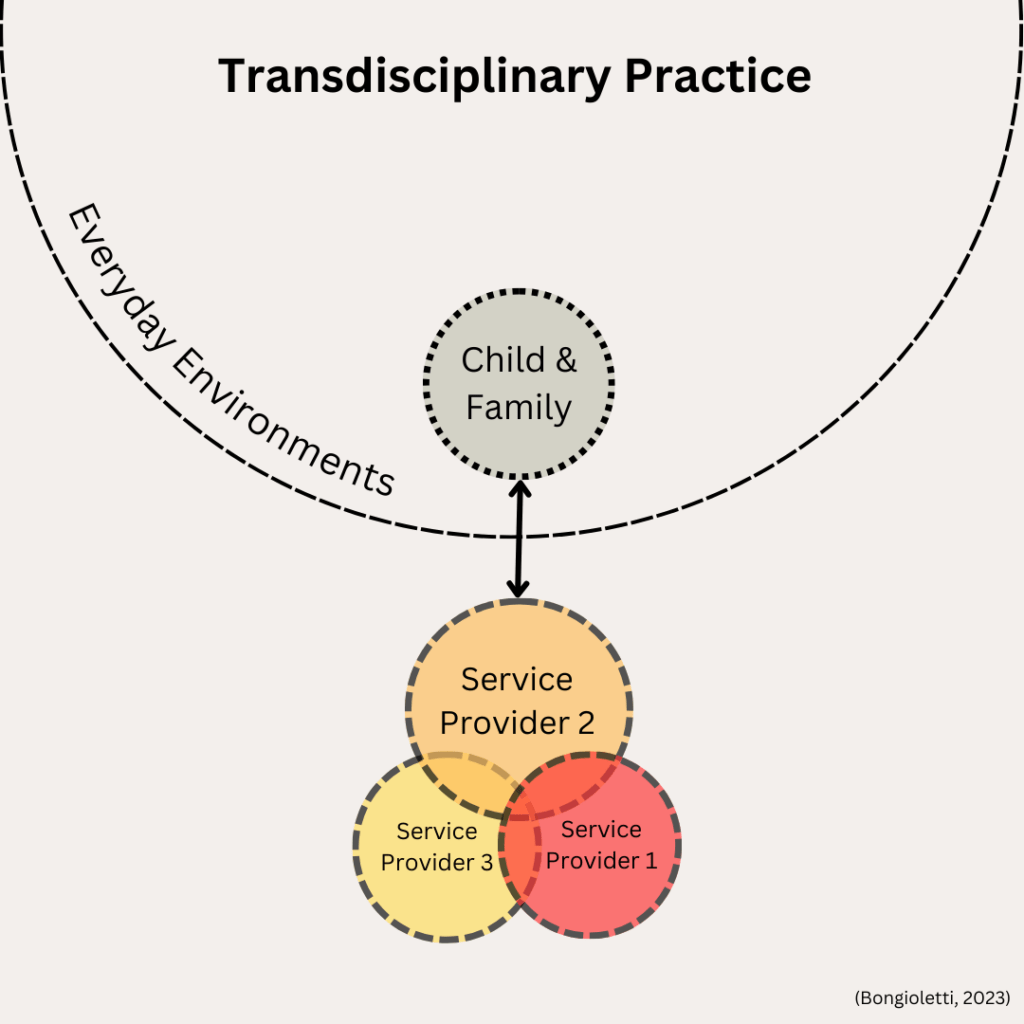
4. Transdisciplinary Practice is where the child and family have a primary relationship with one service provider. This provider takes on a lead role in coordinating and collaborating with other service providers on the team and providing early intervention supports that draw on all disciplines through ‘role release’. Goals are shared, and there is a high degree of collaboration and communication between team members. One benefit of this model is that the family have one key contact who can contribute broad skills and knowledge from the broader team, all while working with the family in their everyday environments.
At the end of the day, there is no ‘one size fits all’ when it comes to which model is ‘best’ for children who are DHH and their families. Service providers should prioritize collaboration and capacity building as key elements of success.
References
- Joint Committee on Infant Hearing. (2019). Year 2019 position statement: Principles and guidelines for early hearing detection and intervention programs. The Journal of Early Hearing Detection and Intervention, 4(2), 1-44. https://doi.org/https://doi.org/10.15142/fptk-b748
- Reimagine Australia. (2016). National guidelines: Best practice in early childhood intervention. https://re-imagine.com.au/practitioner/what-is-best-practice/
