
ACHIEVE Series: Why hearing health matters more than you think
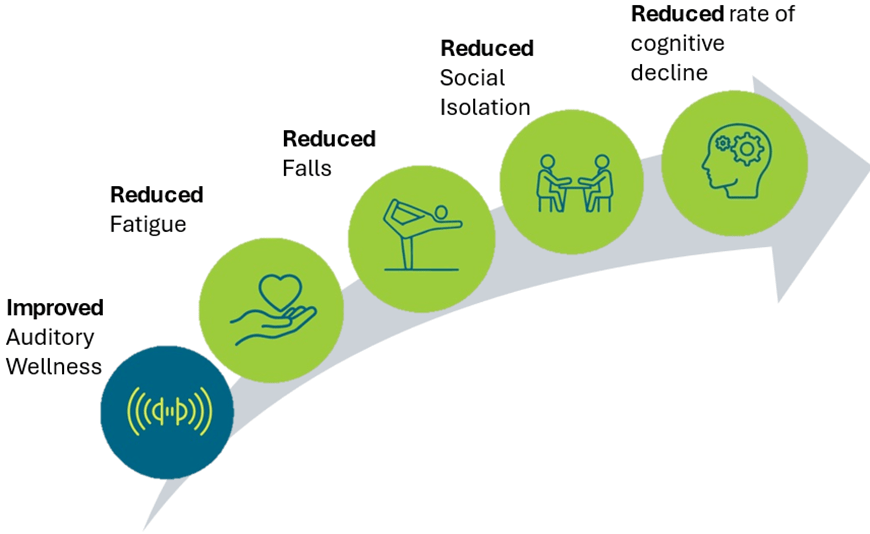
Achieving good auditory wellness can support broader health outcomes. Explore what the ACHIEVE Study findings suggest across overall well-being, and what this can mean for audiologists in clinical practice as well as for those with hearing difficulties.
When we think about well-being, we often picture exercise, nutrition, and mental health. But here’s something that doesn’t get enough attention: hearing health, or “Auditory Wellness”.
Recently, a well-being framework of hearing health defined “Auditory Wellness” as the ability to process sound and fully participate in life without listening-related limitations.1 It’s not just about hearing; it’s about connecting, communicating, and engaging with the world.
Untreated hearing loss isn’t just an inconvenience. It can negatively influence well-being in other parts of life: physical, emotional, social, and even cognitive health.
The good news? Improving auditory wellness can improve overall well-being. And the ACHIEVE Study, among others, offers some of the strongest evidence to date on what changes when best-practice hearing care is provided.

Beyond hearing: Well-being benefits
Hearing health doesn’t stop at your ears. The ACHIEVE Study randomized participants to either a best-practice hearing intervention or a control healthy aging education and measured health outcomes over 3 years. The ACHIEVE study allowed us to compare between groups on multiple dimensions of well-being; including emotional, social, physical, and cognitive, and found some fascinating connections.
- Emotional well-being includes the quality of mood and emotional experiences and the ability to manage these emotions.
Majority of participants in the ACHIEVE study reported an increase in fatigue over 3 years (aging can do that!). However, the group that received the hearing intervention reported less symptoms of fatigue compared to the control group,2 indicating a beneficial effect of improved auditory wellness on fatigue. - Physical well-being includes overall physical health and risk of illness or injury.
The group that received hearing intervention had a 27% reduction in falls over the 3-year period. When listening takes less effort, the brain has more resources for balance and movement. Also, better hearing allows for better awareness of sounds, improving spatial listening. That’s a potentially life-saving benefit.3
- Social well-being includes relationships, communication and connection with others.
Hearing intervention led to significantly lower loneliness scores, larger social networks, and more diverse connections. With improved hearing, people are more likely to join conversations, attend events, and stay socially active.4 - Cognitive and psychological well-being includes memory, attention, executive function and language abilities.
In the overall study, hearing intervention did not significantly slow cognitive decline over three years. However, in a cohort of participants who were at higher risk for dementia, hearing intervention substantially reduced cognitive decline.5 That’s a powerful reason to act immediately.
Together, these findings highlight how hearing health can support broader well-being, not only hearing-related outcomes.
Auditory wellness improves life in big ways
Participants who received the best-practice hearing intervention had remarkable improvements in auditory wellness in the ACHIEVE Study.
- Processing of sound: One way to assess processing of sound is through understanding speech in noisy environments. When wearing hearing aids, the ACHIEVE participants’ ability to understand speech in noise improved by 3.5 dB, when compared to not wearing hearing aids.
- Listening goal attainment: 95% of participants reported improvement in the listening situation in which they most wanted to improve.
- Self-reported residual activity limitations: When asked about their most important listening situation, like communicating with friends or family, participants reported only “slight difficulty” when wearing their hearing aids.
- Self-reported residual participation restrictions: When asked about how much their hearing difficulties affected the things they can do, on average, participants reported being only “slightly affected”, when using their present hearing intervention.
- Self-reported impact of hearing loss: A recommended way to assess auditory wellness is through the self-report measures, like the Hearing Handicap Inventory. At 6 months, there was a significant reduction in hearing handicap, which was maintained across the 3-year study. That is, auditory wellness had improved following hearing intervention but did not improve in the control group.
Check out these ACHIEVE publications for more information about auditory characteristics6, hearing intervention7, and auditory wellness improvements8.
ACHIEVE Study context and design
The Aging and Cognitive Health Evaluation in Elders (ACHIEVE) Study was the first large-scale randomized controlled trial, to evaluate the effect of a best-practices hearing intervention versus a health education control on 3-year trajectory of cognitive decline in older adults with untreated hearing loss.
Nearly 1,000 participants aged 70–84 with untreated mild-to-moderate hearing loss and no substantial cognitive impairment joined the study between 2018-2019 across four study sites in the U.S. (Jackson, MS, Forsyth County, NC, Minneapolis, MN, Washington County, MD).
Participants were split into two groups: one received best-practice hearing intervention, and the other received a health-education intervention.
In practice: What this means for hearing care professionals
The ACHIEVE Study reinforced a practical takeaway message: it can be helpful to track auditory and overall well-being outcomes alongside conventional audiometric and communication outcomes. You might consider:
- Collect measures such as the Revised Hearing Handicap Inventory (RHHI), or other psychometrically valid and reliable patient-reported outcomes, not only hearing thresholds. Check out the freely available 2025 NASEM report9 on meaningful outcomes here.
- Set 2-3 listening goals early, then revisit them at follow-ups to reinforce progress.
- Ask about participation restrictions, activity limitations, social networks, fatigue, and falls as part of holistic counseling, then tailor support accordingly.
The bottom line: Hearing is critical to well-being
Hearing loss is more than an auditory issue, it’s a whole-health issue. As we consider the influence of hearing intervention on a wide range of health outcomes, let’s make sure evidence-based, patient-centered, holistic, best-practice hearing interventions are provided.
Best-practice hearing care isn’t just about hearing better; it’s about living better. And that’s something worth prioritizing.
Source of Funding:
The Aging and Cognitive Health Evaluation in Elders (ACHIEVE) Study is supported by the National Institute on Aging (NIA) grant R01AG055426, with magnetic brain resonance examination funded by NIA R01AG060502 and with previous pilot study support NIAR34AG046548 and the Eleanor Schwartz Charitable Foundation, in collaboration with the Atherosclerosis Risk in Communities (ARIC) Study, supported by National Heart, Lung and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C,HHSN268201100008C, HHSN268201100009C, HHSN268201100010C,HHSN268201100011C, and HHSN268201100012C). Neurocognitive data in ARIC is collected by U01 2U01HL096812, 2U01HL096814, 2U01HL096899, 2U01HL096902, 2U01HL096917 from the NIH (NHLBI, NINDS, NIA and NIDCD), and with previous brain MRI examinations funded by R01HL70825 from the NHLBI. Hearing aids, hearing assistive technologies, and related materials used in the ACHIEVE Study were provided at no cost to the researchers or the participants from Sonova/Phonak LLC. The funders of the study, nor the sponsoring manufacturer, had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Acknowledgments: Members of the ACHIEVE Collaborative Research Group are listed at achievestudy.org. The authors thank the staff and participants of the ACHIEVE and ARIC studies for their important contributions.
References:
1. Humes, L. E., Dhar, S., Manchaiah, V., Sharma, A., Chisolm, T. H., Arnold, M. L., & Sanchez, V. A. (2024). A perspective on auditory wellness: What it is, why it is important, and how it can be managed. Trends in Hearing, 28, 23312165241273342. https://doi.org/10.1177/23312165241273342
2. Bessen, S. Y., Zhang, W., Huang, A. R., Arnold, M., Burgard, S., Chisolm, T. H., Couper, D., Deal, J. A., Faucette, S. P., Goman, A. M., Glynn, N. W., Gmelin, T., Gravens-Mueller, L., Hayden, K. M., Mitchell, C. M., Pankow, J. S., Pike, J. R., Reed, N. S., Sanchez, V. A., . . . Group, f. t. A. C. R. (2024). Effect of Hearing Intervention Versus Health Education Control on Fatigue: A Secondary Analysis of the ACHIEVE Study. The Journals of Gerontology: Series A, 79(11). https://doi.org/10.1093/gerona/glae193
3. Goman, A. M., Tan, N., Pike, J. R., Bessen, S. Y., Chen, Z., Huang, A. R., Arnold, M. L., Burgard, S., Chisolm, T. H., Couper, D., Deal, J. A., Glynn, N. W., Gmelin, T., Gravens-Mueller, L., Hayden, K. M., Martinez-Amezcua, P., Mitchell, C. M., Pankow, J. S., Reed, N. S., . . . Lin, F. R. (2025). Effects of hearing intervention on falls in older adults: findings from a secondary analysis of the ACHIEVE randomised controlled trial. The Lancet Public Health, 10(6), e492-e502. https://doi.org/https://doi.org/10.1016/S2468-2667(25)00088-X
4. Reed, N. S., Chen, J., Huang, A. R., Pike, J. R., Arnold, M., Burgard, S., Chen, Z., Chisolm, T., Couper, D., Cudjoe, T. K. M., Deal, J. A., Goman, A. M., Glynn, N. W., Gmelin, T., Gravens-Mueller, L., Hayden, K. M., Mitchell, C. M., Mosley, T., Oh, E. S., . . . Group, A. C. R. (2025). Hearing Intervention, Social Isolation, and Loneliness: A Secondary Analysis of the ACHIEVE Randomized Clinical Trial. JAMA Internal Medicine. https://doi.org/10.1001/jamainternmed.2025.1140
5. Lin, F. R., Pike, J. R., Albert, M. S., Arnold, M., Burgard, S., Chisolm, T., Couper, D., Deal, J. A., Goman, A. M., Glynn, N. W., Gmelin, T., Gravens-Mueller, L., Hayden, K. M., Huang, A. R., Knopman, D., Mitchell, C. M., Mosley, T., Pankow, J. S., Reed, N. S., . . . Coresh, J. (2023). Hearing intervention versus health education control to reduce cognitive decline in older adults with hearing loss in the USA (ACHIEVE): a multicentre, randomised controlled trial. The Lancet. https://doi.org/10.1016/s0140-6736(23)01406-x
6. Sanchez, V. A., Arnold, M. L., Betz, J. F., Reed, N. S., Faucette, S., Anderson, E., Burgard, S., Coresh, J., Deal, J. A., Eddins, A. C., Goman, A. M., Glynn, N. W., Gravens-Mueller, L., Hampton, J., Hayden, K. M., Huang, A. R., Liou, K., Mitchell, C. M., Mosley, T. H., Jr., … Chisolm, T. H., & ACHIEVE Collaborative Study. (2024). Description of the baseline audiologic characteristics of the participants enrolled in the Aging and Cognitive Health Evaluation in Elders Study. American Journal of Audiology, 33(1), 1–17. https://doi.org/10.1044/2023_AJA-23-00066
7. Sanchez, V. A., Arnold, M. L., Reed, N. S., Oree, P. H., Matthews, C. R., Clock Eddins, A., Lin, F. R., & Chisolm, T. H. (2020). The Hearing Intervention for the Aging and Cognitive Health Evaluation in Elders Randomized Control Trial: Manualization and Feasibility Study. Ear and Hearing, 41(5), 1333-1348. https://doi.org/10.1097/aud.0000000000000858
8. Sanchez, V. A., Arnold, M. L., Garcia Morales, E. E., Reed, N. S., Faucette, S., Burgard, S., Calloway, H. N., Coresh, J., Deal, J. A., Goman, A. M., Gravens-Mueller, L., Hayden, K. M., Huang, A. R., Mitchell, C. M., Mosley, T. H., Jr., Pankow, J. S., Pike, J. R., Schrack, J. A., Sherry, L., … Chisolm, T. H., & ACHIEVE Collaborative Study. (2024). Effect of hearing intervention on communicative function: A secondary analysis of the ACHIEVE randomized controlled trial. Journal of the American Geriatrics Society, 72(12), 3784–3799. https://doi.org/10.1111/jgs.19185
9. National Academies of Sciences, E., & Medicine. (2025). Measuring Meaningful Outcomes for Adult Hearing Health Interventions. The National Academies Press. https://doi.org/doi:10.17226/29104
Author info:
Haley Calloway, AuD, Assistant Professor
Dr. Calloway is an Assistant Professor in the Department of Otolaryngology at the University of South Florida. She is a clinical audiologist and specializes in diagnosing and treating hearing disorders for adult and pediatric populations. She is also a Research Audiologist in the Auditory Rehabilitation & Clinical Trials Laboratory.
Theresa Chisolm, PhD, Professor
Dr. Theresa (Terry) Chisolm is a Professor of Audiology in the Department of Communication Sciences and Disorders at the University of South Florida (USF). Dr. Chisolm specializes in rehabilitative audiology and is a licensed and certified audiologist, with over 40 years of clinical and research experience. Previous research examined the efficacy of a computer-based auditory training program for use post-hearing aid fitting, the benefits of group aural rehabilitation, approaches to auditory rehabilitation for veterans with mild traumatic brain injury, and systematic reviews of hearing-related quality of life outcomes from hearing aid use. Her current role as a co-investigator on the Aging and Cognitive Health Evaluation in Elders (ACHIEVE) Randomized Study has spanned from initial conceptualization to development of the manualized best-practices hearing intervention to implementation and fidelity monitoring with her co-PI colleagues at USF’s Audiology Rehabilitation Clinical Trial’s laboratory (ARCT), Drs. Victoria Sanchez and Michelle Arnold.
LinkedIn: https://www.linkedin.com/in/theresa-chisolm-4234366b/

Victoria Sanchez, AuD, PhD, Associate Professor
Dr. Sanchez is a clinician scientist at the University of South Florida where she provides patient care, teaches and mentors trainees, and conducts research in the Auditory Rehabilitation & Clinical Trials Laboratory.
LinkedIn: www.linkedin.com/in/victoria-sanchez-aud-phd-60009119a

Sarah Faucette, AuD, PhD, Associate Professor
Dr. Faucette is an Associate Professor at the University of Mississippi Medical Center. She serves at ACHIEVE’s Jackson site as the lead research audiologist. Faucette also teaches Audiological Management in the UMMC AuD program and works clinically in adult diagnostics and treatment.
Laura Sherry, AuD, Study Audiologist
Dr. Sherry is a research audiologist in the Department of Otolaryngology-Head & Neck Surgery, Division of Research at the Johns Hopkins University, School of Medicine. Her research interests include the correlation between hearing loss and cognitive decline, as well as improving accessibility to hearing healthcare. Sherry is the lead study audiologist at the Washington County field site for the ACHIEVE study.

Morgan Oktela Fuentes, AuD, Assistant Professor
Dr. Fuentes is an Assistant Professor in the Department of Otolaryngology at the University of South Florida, where she serves as both a clinical and research audiologist as well as the manager of the audiology clinic and research laboratory. Her work spans auditory rehabilitation, clinical trials, and hearing–cognition research, including roles in the ACHIEVE and EARHLI studies. She also serves as a Principal Investigator and Co‑Investigator on multiple institutional and industry‑sponsored projects focused on advancing hearing healthcare and improving patient outcomes.

